Diagnosis of Vulvar and Cervical Diseases Using Colposсopy

Colposcopy is a diagnostic procedure in which a colposcope is used to provide an illuminated, magnified view of the cervix, vagina, and vulva to look for malignant and premalignant epithelium. Malignant and premalignant epithelium have specific macroscopic characteristics relating to contour, color, and vascular pattern that can be identified by the colposcopist for directed biopsy.
Indications for colposcopy include further assessment of cervical cytologic abnormalities or abnormal human papillomavirus (HPV) tests, patients exposed to diethylstilbestrol in utero, patients with gross abnormalities of the lower genital tract, and as an adjunct to surgery of the cervix, vagina, and vulva.
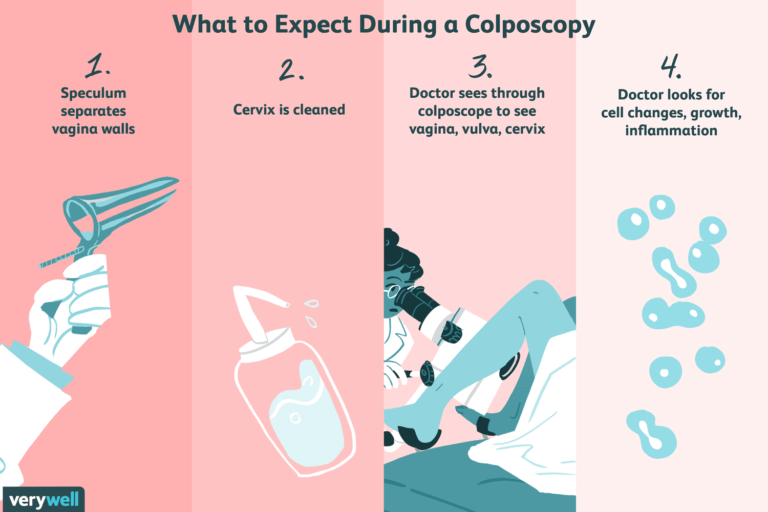
Procedure
- The cervix and vagina are examined with a bright light and then with the colposcope. Pigmented areas and obvious lesions are noted. Three to 5 percent acetic acid is applied to the cervix and the cervix is reexamined.
- Metaplastic cells, dysplastic cells, and cells infected with HPV reflect light and thus appear white.
- Areas of white epithelium are further evaluated for abnormal vascular patterns, such as punctation, mosaicism, or abnormally appearing vessels.
- The most abnormally appearing areas are biopsied. Biopsies are relatively contraindicated in patients on anticoagulation medication, who have a known bleeding disorder, or who are pregnant. (
- Colposcopy by an experienced colposcopist will usually detect patients with significant disease (ie, high-grade squamous intraepithelial lesion [HSIL], cancer), but some patients with a normal colposcopic examination can still have a significant histologic abnormality. For this reason, it is important to reconcile the cytologic, colposcopic, and histologic findings in formulating a diagnosis and management plan for each patient and following these patients closely.